Many Symptoms, One Brain: Different Forms of Pain Trace Back to the Same Source
Neuroplastic symptoms consist of ongoing pain or illness that is caused by nerve pathways in the brain, rather than disease or structural injury. These symptoms manifest in many different ways, including back pain, headaches or migraines, chronic fatigue, digestive or bowel problems, and more. It is also extremely common for people to have multiple symptoms. In our recent nationally representative study of US adults, for example, we surveyed a subgroup of the population that we identified as being highly likely to have neuroplastic symptoms. In this group, we found that 71% reported two or more symptom types.
Because these symptoms are often very different from one another, it might lead people who are experiencing these different symptoms to think that they are completely unrelated. Consider someone who has chronic foot pain and recurring migraines. From a purely physical perspective, it does not make sense that these different symptoms could be related. However, when we understand both types of symptoms as neuroplastic, we can better understand how the brain is likely to be causing both symptoms.
How can we be confident that such a wide variety of different symptoms can have the same cause? The first step is evaluating how often certain symptoms co-occur, and comparing this to what we would normally expect if the symptoms were not related. Consider another example where someone has ongoing back or neck pain as well as headaches/migraines. In the US, we estimate from our survey data that about 31% of adults have ongoing back or neck pain, and about 17% have recurring headaches/migraines.
These symptoms co-occur more than twice the amount that we would expect to happen by chance alone. If these two symptom types were totally independent, we would expect to find them happening together in about 5% of the population (0.31 ✕ 0.17 = 0.05). But when we examine this in our data, we find these symptom types happening together in 12% of the population—far more than the expected prevalence. We see even stronger evidence of connections between many other combinations of symptoms.
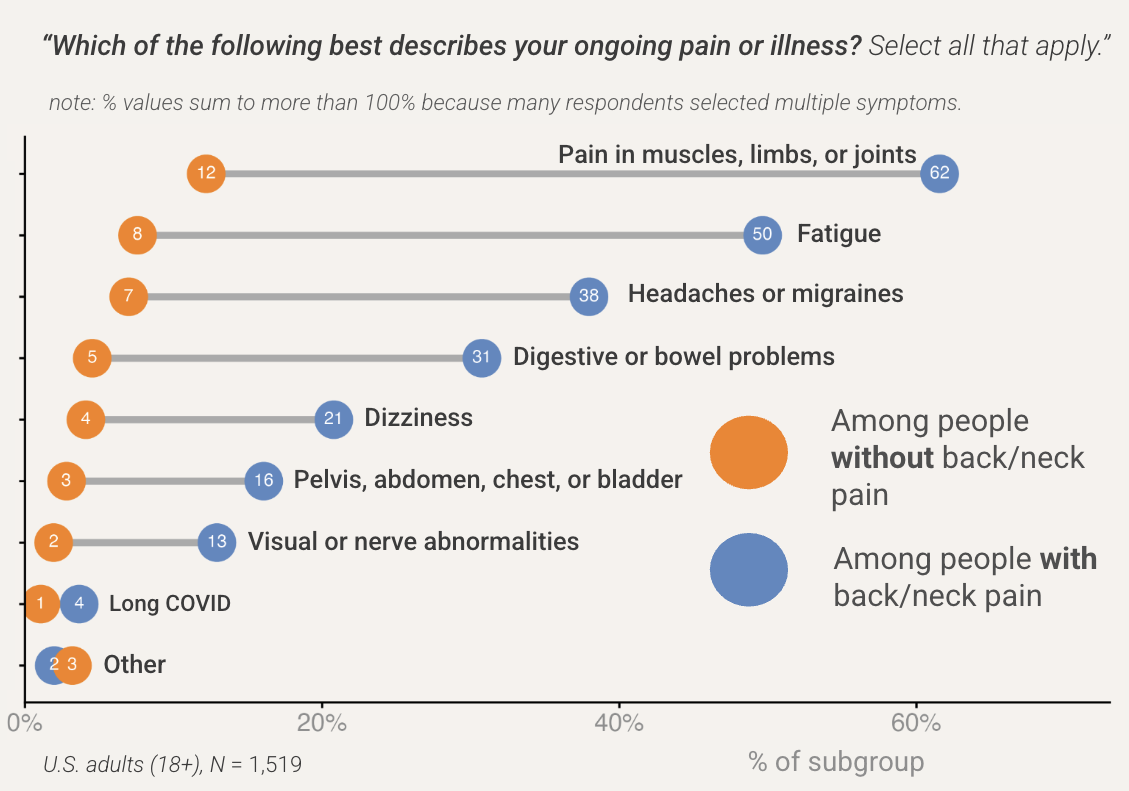
Another way to think about this is: “If someone has symptom A, what are the chances they have symptom B?” Consider Figure 1 below. We took our national survey sample and put people into one of two groups: those who reported having back/neck pain and those who did not. We can see that knowing whether someone has back/neck pain or not tells us a lot about the chances that they have other symptoms. Our findings show, for example, among people with back/neck pain, 50% also have chronic fatigue. But among people without back/neck pain, only 8% have chronic fatigue.
Figure 1: People with ongoing back/neck pain are extremely more likely to have additional symptoms
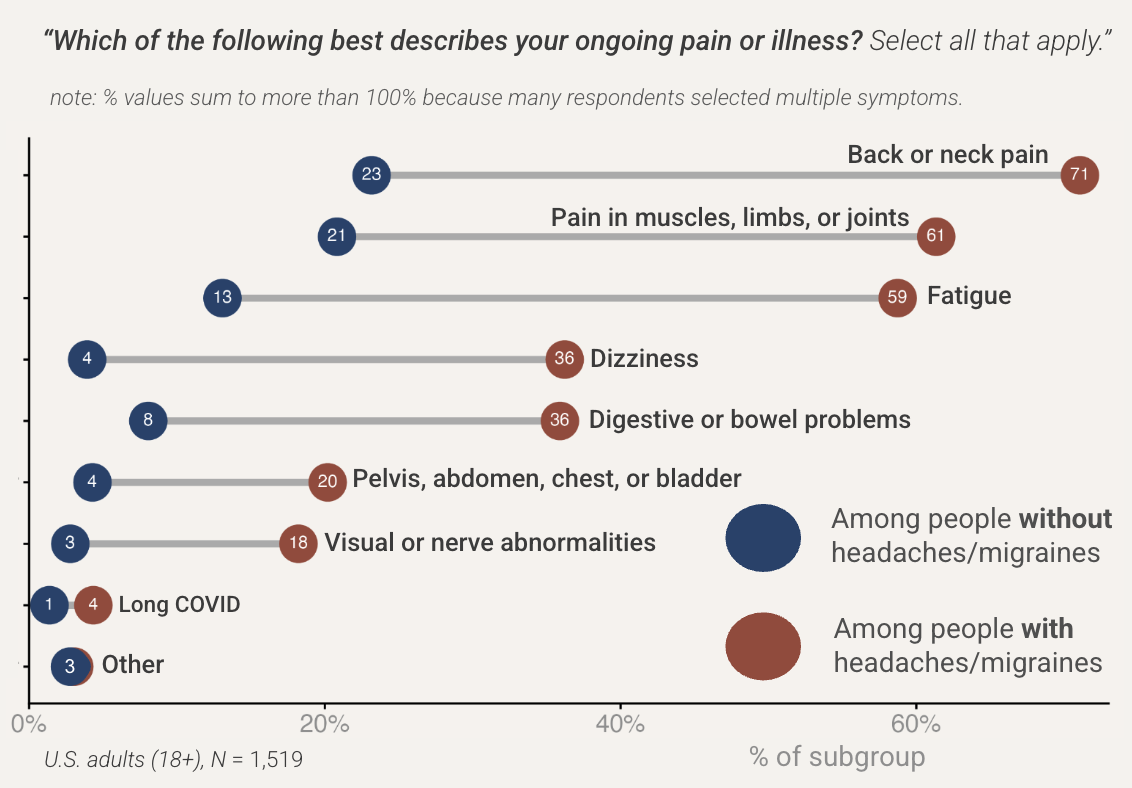
We took the same approach in Figure 2 below, but this time we grouped people by whether they reported having chronic headaches or migraines. We see a similar pattern in which people who have headaches/migraines are much more likely to have other symptoms than people who do not have headaches/migraines. Together, these findings demonstrate strong connections between different symptoms.
Figure 2: People with ongoing headaches/migraines are extremely more likely to have additional symptoms
Coming back to the question of whether different symptoms have a common cause, these findings are certainly suggestive, especially when people experience different symptoms that cannot be explained as being structurally related to each other. But this evidence alone is incomplete. Our case gets significantly stronger if we could treat the key underlying cause and see improvements across different kinds of symptoms. For example, if psychological treatments can lead to substantial improvements in foot pain as well as migraines, back pain, or digestive problems, we can be more confident of the common cause hypothesis.
This is indeed what we find. More and more evidence is accumulating that shows many different physical symptoms improving significantly from purely psychological approaches. Some notable examples are randomized controlled trials on Pain Reprocessing Therapy and Emotional Awareness and Expression Therapy. What is so amazing about these therapies is that they can treat such a wide variety of symptoms.
When we put all of this evidence together, we gain a much clearer understanding of the path to recovery from neuroplastic symptoms, which includes calming the nervous system, processing emotions and life challenges, and related therapeutic approaches. An important challenge now is to build awareness––among practitioners and the general public––of the fact that the brain can be a common cause of symptoms that are seemingly unrelated. If we can build this awareness, many more people would be able to successfully recover from their ongoing pain or illness.
If you connect with this, or know others who might, join us in advancing a national conversation about neuroplastic symptoms, their true causes, and the real possibility of recovery. Become part of the effort to reshape how ongoing pain and illness are understood and treated. Together we can make recovery a real possibility for millions who are needlessly suffering. Learn more here about the community of people helping to spread awareness.
Matthew Goldberg, PhD, and Abel Gustafson, PhD, are Co-founders of XandY—a research and communication strategy firm. David Clarke, MD, is President of the Association for Treatment of Neuroplastic Symptoms. Monique Sondag, BS, is the Strategy and Development Director at the Association for Treatment of Neuroplastic Symptoms.